The Affordable Care Act Implementation
Abstract
The Patient Protection and Affordable Care Act was an ambitious program meant to ensure that every American legal resident can have access to quality healthcare services irrespective of their social status. For a long time, the country had been struggling to enact a policy that would lower the cost and increase the accessibility of healthcare services to the masses. ACA promised to deliver that goal in the most effective way possible. The program was funded through a new tax that individuals, companies, and government entities had to pay. The goal of universal health insurance coverage was to ensure that every hospital is compensated for the services that they offer to Americans. Implementation of the program has faced numerous challenges, but most states have already embraced it. Only 12 states are yet to fully implement the program. Information gathered and processed in this study shows that the program has made quality healthcare services available to Americans, especially those with low incomes.
Background and Contextual Information of the Program
Introduction
The Patient Protection and Affordable Care Act, often known as the Affordable Care Act (ACA) and widely nicknamed Obamacare, focuses on expanding health insurance coverage to the poorest of Americans to ensure that quality healthcare is available to all legal residents of the country irrespective of their social status. It is important to understand the background of this program. Dawes and Williams (2020) explain that the political elites, especially the Democrats, had been trying to create a universal healthcare program for over 70 years before the ACA bill was introduced. When President Barack Obama came into office, one of his priorities was to make a reality program that would ensure that all legal residents have access to quality medical cover, including those whose earnings were too low to afford to pay for private health insurance cover.
The bill was introduced in Congress in 2009 and President Obama personally addressed the legislators, explaining the benefits that it would offer. The bill faced fierce resistance from Republicans in both houses, who argued that it was a socialist idea that went against the basic principles of capitalism that the United States has always fought for (O’Dowd & Charbonneau, 2021). Some scholars have argued that the major rift was primarily caused by political differences between the two major parties, not the principles and the spirit of the law. It was finally approved despite the challenges; the bill was passed in the Senate on December 24, 2009, and in the House on March 21, 2010. The bill was signed into law on 23 March 2010, and the provisions of the law went into effect on January 1, 2014 (Chies & Pratt, 2020). It has introduced major changes which have made healthcare accessible to most Americans.
The target audience of the program was the general American population through their representatives in Congress and the Justice System. The goal of this program was to ensure that no American citizen or legal resident would be denied access to medical care because of their inability to pay. It created a universal healthcare program based on the premise that this is a basic need. The objective of the drafters of this program was to ensure that basic healthcare does not become a preserve of the rich.
The purpose of ACA was to ensure that large companies and the rich would help shoulder the cost of healthcare for the poor. The mission was to ensure that everyone made their contribution to the program, based on their level of income, to shoulder the burden of healthcare. The primary philosophy of the drafters of this law was that basic health, just like security, was a basic human need, without which one can die of a preventable disease. As the government remains committed to providing security to all Americans regardless of their social status, it is equally a moral responsibility to ensure that basic healthcare needs are provided. The staff capacity or personnel responsible for the implementation of the program varies from one state to another (Hill & Hupe, 2014). It cannot be clearly defined because of the complex nature of the program’s implementation, especially after the major changes President Trump introduced when he came to power.
Critical Features of Implementation
The Affordable Care Act was landmark legislation in the United States as the country had struggled for over seven decades to enact a policy that would ensure that all citizens get basic healthcare coverage. The bill faced fierce opposition in Congress but the Democrats used their numbers both in the Senate and the House to ensure that it passed. As Obama (2017) explains, passing the bill was just one milestone in this program. Implementation was the major challenge that it faced as soon as it was signed into law. Despite its wide acceptance among a section of Americans, the initial challenge was funding the program. It meant that the government had to introduce new taxes, which would increase the cost of doing business in the country and the overall cost of living for the American public. The new levy has been the primary concern that has led to the slowed implementation and outright rejection of the program. It is necessary to assess the critical features of the implementation of the program.
Program’s Activities and Procedures of Operations
The bill went through intense lobbying as the Obama administration made an effort to ensure that it was passed in Congress. On December 24, 2009, the bill passed the Senate 60-39 after getting the support of all the Democrats. The bill was then sent to the House, where it passed on March 21, 2010, by a vote of 219–212 (Hicks, 2020). Two days after the bill passed the Congress, President Barack Obama signed it into law on March 23, 2010 (Hicks, 2020). Figure 1 below shows President Obama signing the bill into law in presence of members of Congress and other guests. Once it became a law, it became essential for the government to ensure that it is implemented as was intended by its drafters. It is necessary to discuss critical features of its implementation. Assessing the program’s activities and procedures of operation is essential at this stage.

Critical Features of the Program’s Implementation
The Affordable Care Act had critical features that defined its implementation. Day (2020) explains that ACA was a major milestone that was made in the healthcare sector to ensure that there was universal coverage. One of the critical features of this program’s implementation is that it is primarily funded through a new tax. The Act introduced tax provisions that targeted business entities, individuals, families, government institutions, and tax-exempt organizations (Beik & Pepper, 2014). The goal was to create a large pool of resources that would help fund healthcare in the country. The drafters of this law believed that creating a large revenue stream to fund the program would ensure that every legal resident in the country could access quality healthcare. This feature, which forms the basis of the program, is considered the most undesirable by most of the American population, especially those who feel that implementing the program comes at a high cost to the middle and upper-class members of society.
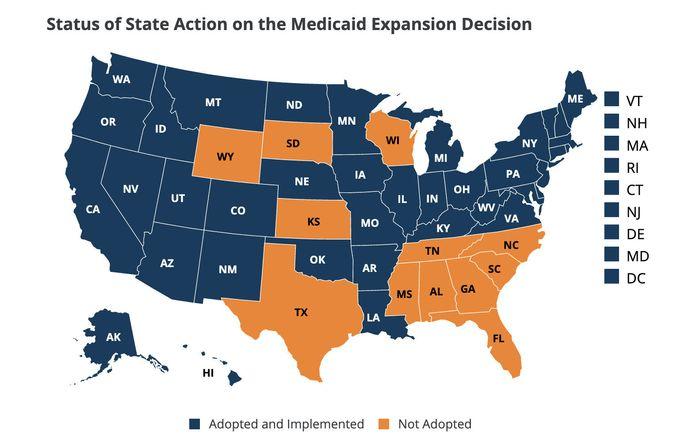
The Obama administration introduced a new feature of the ACA to help in promoting its implementation. The federal government introduced an incentive for states that implemented the program in 2014. In this plan, individual states received a 100% match for the implementation of the program (Raudenbush, 2021). It meant that the federal government would match the investment that every state made in implementing the program. This was a major incentive for individual states who saw an opportunity to expand their healthcare sector through the direct support of the federal government. Although the match rate has reduced to 90% in 2021, it is still a major incentive for the states. Only 12 states are yet to fully implement this program, which means that they are losing the benefits the federal government is offering.
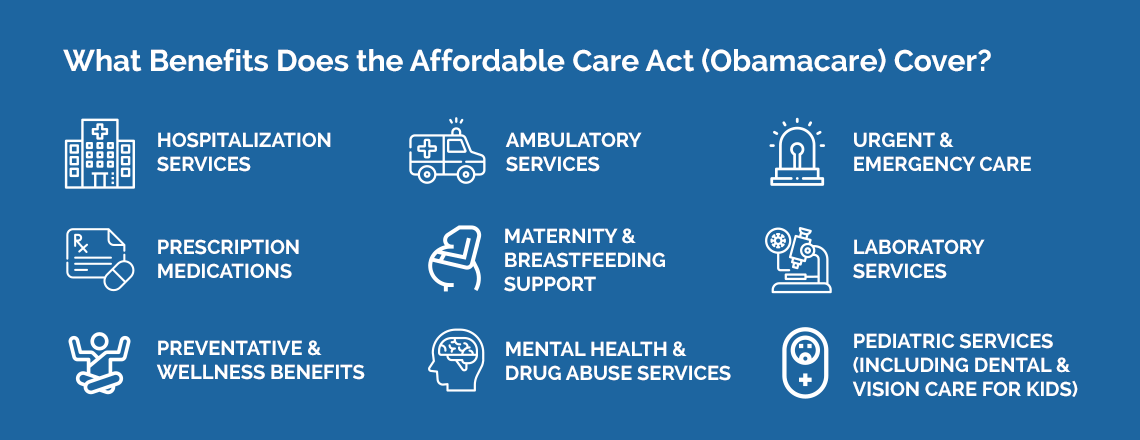
The program was designed to be implemented at the state level instead of the federal level. According to Perricone (2020), each state has full control of all the medical facilities within its jurisdiction. Laws, regulations, and management of healthcare institutions, including medical insurance coverage, vary from one state to another in the country. As such, the program had to be handed over to each state for implementation. The Act provided basic guidelines that each state had to adhere to during implementation. The states also had the responsibility of adjusting their existing policies and programs in the healthcare sector to accommodate the program. They had to help in collecting the tax and in using the resources to make accessible affordable healthcare to their legal residents. Figure 2 below shows the healthcare services that are covered under this universal health program.
When implementing a program, it is always essential to define the materials needed to make it a success. The implementation of ACA is unique relative to other programs, especially those in the construction sector. According to Stanhope and Lancaster (2021), ACA does not directly involve constructing more hospitals. The primary goal is to ensure that hospitals in the country, especially public healthcare institutions, do not turn away patients because of their inability to pay.
The primary material for the implementation of this program is money needed to compensate individual institutions for the care they offer to patients. These healthcare institutions may need to expand their physical structures to meet the expected demand (Rundio, 2021). As the services become more affordable to the masses, the number of people visiting hospitals may increase. Given the fact that these institutions are effectively rewarded for the services that they offer, they may find it reasonable to expand their capacity. However, the provisions of ACA only require the institutions to ensure that their services meet the set standards. In case the services can be offered using the current structures and equipment, these institutions are not required to expand.
The budgetary allocation is another major issue that has to be considered when implementing a new program. ACA was an ambitious program meant to ensure that the government made available, affordable healthcare. However, the team acknowledged that the implementation would be expensive. According to Rosenthal (2020), the Center for Medicare and Medicaid Innovation was created and appropriated $ 10 billion each year, from FY 2011 to 2019. The institution was meant to supervise the compensation of healthcare institutions in each state that were part of the program. ACA appropriated an additional $11 billion to the Community Health Center Fund, primarily focused on financing rural healthcare institutions involved in the program (Porsche, 2021). The money was meant to help expand these community health centers across the country on a state-by-state basis. From FY 2010 TO FY 2019, ACA has appropriated more than $100 billion, of which $40 billion was allocated to the State Children’s Health Insurance Program (Crotty, 2021). The author notes that the federal government is required to continue supporting this program through various provisions provided within the law.
Site location is an essential factor that has to be defined when implementing a program. ACA was a federal law that affected all states in the country. However, its implementation evolved, with each state having the ability to choose when to introduce it (Crotty, 2021). The devolution of the implementation of the program was essential because each state has its unique healthcare system. They had to reform their healthcare systems to match the requirements of the new law. The implementation was further devolved to districts across the states. Individual hospitals within the participating states had to embrace the new system. These individual institutions were expected to redefine the payment programs for their patients. They had to allow patients without private insurance coverage to use their services as long as they were legal residents of the state. They would then be expected to bill the new universal health insurance coverage to ensure that they are compensated for the services that they offer. The new program also meant that private health insurance companies had to redefine their products in line with the new changes introduced by ACA.
Provisions Were Made For Assessment and Reporting
The federal government had to develop an effective provision for assessing and reporting the progress in the implementation of the program. The implementation team of ACA identified specific barometers that had to be used in assessing the readiness of the relevant stakeholders to implement the program. One of them was to assess if the marketplace was fully functional and ready for ACA. The Commonwealth Fund Affordable Care Act Tracking Survey was tasked with determining if people were signing up for the program (Oberlander, 2019). It was also focused on determining if institutions responsible for the implementation were capable of undertaking their respective activities.
Assessing whether people enrolled in the new coverage was another way of assessing the progress of the program. The Congressional Budget Office has the data that shows the number of people who have signed up and are actively using the program. Recent data shows that millions of Americans have enrolled in the program, which is a sign of good progress made (Goozner, 2017). The number of uninsured legal residents in the United States has drastically dropped since the enactment of this law. It is also necessary to assess the quality of insurance coverage that is offered. Butler (2017) explains that it is important to reduce cases of underinsurance as more people get to be covered. The out-of-pocket cover should reduce while the number of services offered under the new cover should be high. Assessment should show that ACA has been successful in offering basic healthcare services to residents.
Another barometer for assessing the success of the program was to determine if people are using their new insurance when seeking healthcare services. It was expected that once introduced, the number of people who rely on private health insurance coverage in the country will reduce significantly. Data from the health insurance sector in the country show that the usage of this cover largely depends on one’s financial capacity. The upper-middle-class and the rich still have and fully rely on private health insurance coverage. They rarely use the ACA program although they are directly responsible for its funding (Béland et al., 2018). On the other hand, the majority of the poor currently rely fully on ACA to have access to the medical services that they need.
The primary aim of the program was to help lower or at least moderate the growing cost of healthcare in the country. It was meant to control costs and increase the affordability of these services. A survey indicates that although the ACA program has made these services accessible, the issue of the cost of healthcare is yet to be addressed. The program was successful because the poor can now access healthcare services, which are subsidized by both the state and federal governments (O’Dowd & Charbonneau, 2021). However, the cost of care has been rising consistently over the years. It means that if the program is terminated and every American is forced to finance their healthcare, a vast majority of the lower middle class and the poor may not have access to this basic need.
The final barometer is the overall quality of health care that is available in the country. According to Obama (2017), making healthcare services available for the masses comes at a great cost. If proper measures are not taken, quality may be traded for quantity. Local healthcare institutions may be overwhelmed by the high number of patients and they may be unable to offer the best services to the customers. This was an issue when the program was initiated, but it has since been effectively addressed. To reduce congestion at public hospitals, private hospitals were also included in the program. It means that one could easily visit a private clinic and get quality services without having to spend extra money. State governments have also expanded their healthcare facilities in terms of structures and staff to meet the expanded demand. These steps have helped in ensuring that the quality of services provided is not compromised.
Challenges Facing the Affordable Care Act Implementation
The implementation of the Affordable Care Act has faced numerous challenges since its inception. According to Rice et al. (2014), one of the main challenges that were faced in the implementation of the program was a massive misconception. A section of the political class opposed to the program used their influence to spread misleading information to the masses. One of the common misleading messages that were spread during the initial stages of the implementation was that ACA was meant to overtax hard-working Americans to benefit lazy individuals who are earning minimum salaries. A section of the American society was made to believe that this program was leaning towards communism, where resources would be taken from the rich and given freely to the poor. The message created massive opposition to the program, especially among the rich and the middle class who felt that they can afford to pay for the private medical insurance cover. The rejection of the program by a wide section of society forced some politicians to reject its implementation as a way of protecting their political offices.
The Tea Party movement within the Republican Party emerged as the strongest opposition to the implementation of the bill. It partnered with advocacy groups, large companies, and labor unions to reject its implementation (Oberlander, 2019). Labor unions felt that the contributions made by their members would drop significantly because of the deductions made by their members. Companies felt that the law introduced new levies that significantly increased the cost of their operation in the country. Advocacy groups were acting in the interest of major companies and financiers in the country. They all opposed the full implementation of the program, arguing that it denies American citizens the ability to choose the appropriate medical cover that they deserve and can afford. Figure 3 below shows a section of members of the society protesting against the program at a political rally.

The biggest threat to the implementation of the ACA was the unsupportive administration of President Donald Trump. The president had promised his supporters that when elected, he would repeal and replace the bill (Oberlander, 2018). When he took office, one of the changes that he focused on introducing was the abolishment of the program. When it failed to pass through Congress, the president made an executive order that eliminated the federal tax penalty on companies and individuals who violated the policies defined by the program. It meant that entities that failed to remit the necessary payments for the program would not be subject to any fine. Eliminating the fine meant that individuals and companies lacked the incentive to ensure that they make the monthly payments needed to implement the program.
The divisive politics in the United States is largely considered the main reason why the implementation of ACA has faced numerous challenges. From the onset, the bill was viewed as a contest between Republicans and Democrats. In the Senate, all Republicans rejected the bill except one senator who opted not to vote. In the House, all the Republicans present voted against the bill (Butler, 2017). The stage was set, and although the bill was passed because of the superior number of Democrats in Congress, it became a context between the two factions. Since then, Republicans have been making an effort to repeal and replace the Act primarily as a show of power. It means that there is little focus on the benefits of the program to the Americans.
When efforts to repeal and replace ACA failed, some stakeholders opted to fight the program in court. National Federation of Independent Business v. Sebelius, Little Sisters of the Poor Saints Peter and Paul Home v. Pennsylvania, and King v Burwell are some of the notable cases that were presented to the Supreme Court of the United States (Shaw et al., 2021). Other notable cases included the United States House of Representatives v. Azar, California v. Texas, and Maine Community Health Options v. The United States (Stanhope & Lancaster, 2021). Critics of the program made an effort to use the justice system to thwart the implementation of the program. It is important to note that although the courts rejected attempts to abolish the implementation of ACA in its entirety, some of the rulings affected some aspects of the act.
The confrontation between Congress and the federal government threatened the implementation of the program in 2013. The House Republicans accused the president of using executive orders to help ensure that the Act was implemented across the country without the approval of the government (Rice et al., 2018). As such, the House made an effort to defund its implementation as a way of forcing negotiation with the federal government. The decision led to the government shutdown from October 1 to 17 in 2013. The efforts to make major changes or introduce restrictions to the implementation of the bill by the House Republicans were only stopped by the Democratic Senate (Goozner, 2017). The constant fight among arms of the government meant to facilitate effective implementation of the bill has affected the progress of the program.
Analysis and Discussion
The implementation of the ACA was as challenging as the process it took to pass the bill into law. According to Beik and Pepper (2014), the nation has been divided about the benefits and implementation of the program. The rhetoric of the political class has only made it worse as they try to gain political mileage out of this divisive issue. A section of American society still views this program as a socialist strategy where those who work harder and earn higher income have to pay for the healthcare of those who are perceived to be less hardworking. As such, it has remained a relatively less popular policy among the rich and the upper-middle class who view it as an unnecessary burden. A study by Shaw et al. (2021) revealed that the majority of the rich in the United States are not using this universal health insurance coverage, instead opting to use other private health insurance coverage. Consequently, the rich and the upper-middle class are paying for something that they do not use. It explains why they have vehemently opposed the implementation of the program.
On the other hand, the lower middle class and poor Americans feel that the ACA is one of the best healthcare programs that the nation has ever enacted in the last century. For a long time, these citizens have been grappling with the ever-increasing costs of healthcare. It had reached a level where most of them only opted to go to the hospital when their condition became life-threatening because they had to choose between food, clothing, and housing on the one side and medication on the other (Rosenthal, 2020). Seeking medication when the medical condition has advanced meant that more Americans were putting their lives at risk. The program addressed a basic need that was increasingly getting out of reach for many citizens.
Application of Theory
The implementation of the ACA has encountered numerous challenges since it was enacted into law. The perception that the idea is socialist is misleading and has caused some people to oppose its implementation. The analysis shows that 12 states, shown in figure 4 below, are yet to implement the program because of the belief that it is unpopular and less desirable even among the low-class members of society. The problem, as Crotty (2021) observes, is that the public has been misled into believing that the law is meant to benefit a few lazy individuals at the expense of the hardworking majority. Theory of action can be instrumental in guiding the implementation of this program among those states that are yet to embrace it.
As shown in Figure 5 below, the first step when using this theory is to define the problem. In this case, the problem is that the majority of low-cost households cannot afford quality healthcare services. Some of them are forced to wait until their condition becomes critical before visiting the hospital (Rosenthal, 2020). A new program has been introduced by the federal government, which is meant to provide medical cover to these less fortunate members of the society in the form of ACA. The problem is that this policy is unpopular among a section of the society, which means that its implementation may make the local politicians, especially the governor, less popular. However, it addresses a major need in the local community because health is a basic need. The local government should prepare the locals, using Kurt Lewin’s model discussed below, to help reduce resistance among the locals.
The second step is to plan and undertake specific activities relevant to the implementation of the program. The federal government clearly defined activities that are needed to implement the program (Dawes & Williams, 2020). An overwhelming majority of states in the country have also implemented this law. The remaining states can easily embrace best practices from the states that have implemented the program and follow their blueprint. When defining the activities, they have to take into consideration factors that are unique to the state, such as the population of those who will likely benefit from the program, expected revenue from the tax, availability of staff to meet the extra demand and the capacity of the existing systems and structures at the local hospitals. Once these factors are defined, the state can then introduce the program.
The next step is the assessment of the outcome of the program. The team will assess the short-term outcome within the first few months of introducing the program. It will involve assessing how well the healthcare facilities are coping with the expected increase in the number of patients (Hill & Hupe, 2014). The assessment will also involve determining how well these facilities meet the expectations of their clients. The focus will be to identify specific challenges that these institutions are facing and find ways of addressing them. The relevant authorities will then assess the long-term outcomes of the program. Factors such as the number of patients seeking medical attention at the right time, reduction of common ailments, and revenue flow to continue supporting the program are some of the long-term outcomes that should be assessed.
The final stage is the review and a possible revision of the program. Each state faces unique challenges, such as the number of illegal immigrants, the population of low-income households, the number of those in gainful employment who can contribute to the program, and the number of companies expected to contribute to the tax program (Chies & Pratt, 2020). It is expected that each state will revise the program upon a periodic review, to meet specific expectations based on the realities that they face.

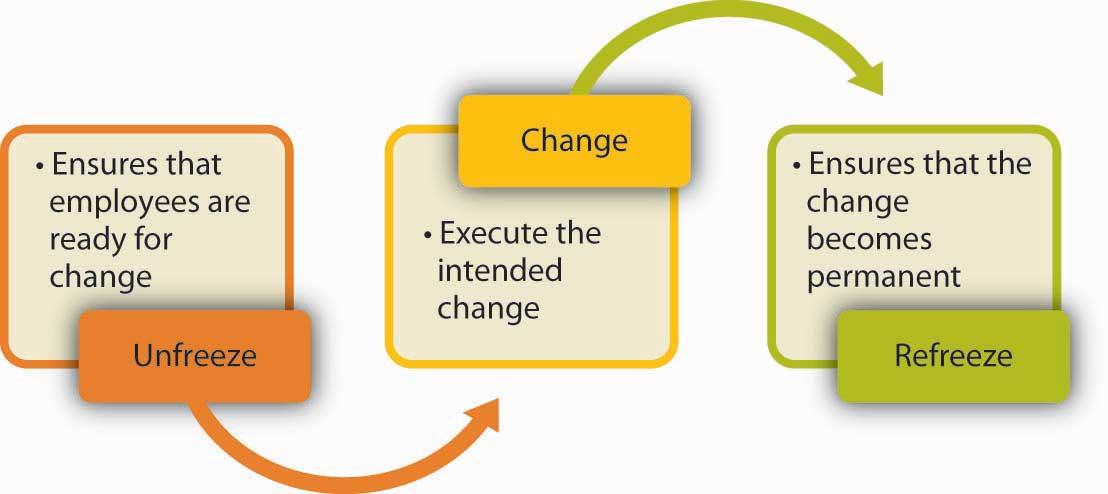
When introducing change in an organization or a state, as is in this case, it is always important to use a strategy that will minimize resistance among stakeholders as much as possible. Figure 6 below shows Kurt Lewin’s theory of change that can be used to adequately prepare stakeholders and ensure that they are ready for the change. The first step is to unfreeze, which involves preparing the stakeholders for the expected change. The policymakers and the state government should explain the reason why it is necessary to implement the program and how it intends to benefit the masses. Employees who are directly expected to implement this program should be prepared and informed of the new role that they are expected to play.
The second stage is the actual introduction of change when the stakeholders are fully prepared. As Day (2020) observes, the stage involves the execution of the intended change. In this case, the state will introduce the ACA and require all the companies, state agencies, and individuals to start making their contributions as defined by the law. The hospitals will be expected to start accepting patients who are covered by the program and to offer them all the services shown in figure 2 at no cost. The last stage is to refreeze, which involves ensuring that the introduced change becomes permanent (Chies & Pratt, 2020). The state authorities will ensure that all the parties involved play their respective roles to ensure that the program is a success.
Policy/Political Intervention of the Program’s Implementation
The implementation of this program was meant to address a serious issue in the United States’ health sector. The increasing gap between the rich and the poor had led to cases where a section of the society could not afford medical services. The ACA was seen as a major policy change that would effectively address the problem. It did not focus on addressing the entire economic problem. Instead, it focused on ensuring that all Americans and legal residents could afford basic healthcare regardless of their income. The legislation was lauded as a major shift from the traditional policies that required everyone to shoulder the burden of their income (Raudenbush, 2021). However, the discussion above shows that it has faced numerous challenges as a section of society feels that it is a socialist idea.
Those who are opposed to its implementation have tried various approaches to overturn the program. Attempts to repeal and replace the law through Congress, especially by members of the Republican Party, have failed. As such, the court remained the only option that they could use to redress the problem. However, all the cases that were presented to the Supreme Court have equally failed to eliminate the law. The only successful attempt that was made against the law was the executive order that was Executive Order Promoting Healthcare Choice and Competition of 2017, signed by President Trump, which eliminated all fines levied against entities that failed to make contributions to the program (Hicks, 2020). It was aimed at denying the program the finance it needed and letting it die without any other piece of legislation.
The House has made several attempts to have this program repealed and replaced. In 2011, the House passed the Repealing the Job-Killing Health Care Law Act 245-189 (Perricone, 2020). However, it was shot down when it was taken to the Senate, where the Democrats still had a significant influence. On February 3, 2015, another effort was made by the House to repeal and replace the program, and it passed 239 to 186 (Chies & Pratt, 2020). However, it failed to achieve its goal despite getting the approval of the majority of the House members. It was the record 67th time that the Republican politicians made an attempt and failed to repeal and replace the law.
The current administration of President Joe Biden, a Democrat, is seen as being friendly to the program. This administration will likely roll back some of the efforts made by the previous administration that focused on frustrating its implementation by denying it the much-needed resources. The current atmosphere in the political arena is seen as being supportive of this program. The Democrats have managed to gain control of the House, the Senate, and the White House (Executive), which means that it is less likely that a bill against ACA can be passed. The program still needs political goodwill to ensure that it remains successful.
Conclusion
The Affordable Care Act was an outcome of a long debate about how well the government could ensure that every American has access to quality healthcare as a basic need. As discussed in the paper, the cost of healthcare had been consistently increasing in the years preceding the enactment of the law. It had become almost impossible for low-income families in the country to afford these services. Some would have to choose between paying for food and paying for medical services. In many cases, they would opt to avoid seeking medical services until their condition became unbearable. Some would lose their lives because of the problem of coming to the hospital when it is too late to manage their condition.
The introduction of the ACA was a major relief to families that could not afford to pay the increasing costs. Since its introduction, it has been reported that many people are seeking medication at the right time, making it easy to manage their condition. The program has helped in solving a major problem that was threatening to worsen the problem of income inequality in the country. With political goodwill, this program will help in ensuring that every American citizen and legal immigrant has access to medical services regardless of their financial status.
References
Beik, J., & Pepper, J. (2014). Health insurance today – ebook: A practical approach. Elsevier Health Sciences.
Béland, D., Rocco, P., & Waddan, A. (2018). Obamacare in the Trump era: Where are we now, and where are we going? The Political Quarterly, 89(4), 687-694. Web.
Butler, M. (2017). Repeal and replace Obamacare: What could it mean? JAMA, 317(3), 244-245. Web.
Chies, S., & Pratt, J. R. (2020). Pratt’s long-term care: Managing across the continuum. Jones & Bartlett Learning.
Crotty, W. J. (Ed.). (2021). The presidential election of 2020: Donald Trump and the crisis of democracy. Lexington Books.
Dawes, D. E., & Williams, D. R. (2020). The political determinants of health. Johns Hopkins University Press.
Day, R. (2020). Marching toward coverage: How women can lead the fight for universal healthcare. Beacon Press.
Goozner, M. (2017). The many consequences of repealing Obamacare. Challenge, 60(2), 122-140. Web.
Hicks, L. (2020). Economics of health and medical care. Jones & Bartlett Learning.
Hill, M. J., & Hupe, P. L. (2014). Implementing public policy: An introduction to the study of operational governance. Sage.
Nistelrooij, A. (2020). Embracing organizational development and change: An interdisciplinary approach based on social constructionism, systems thinking, and complexity science. Springer.
Obama, B. (2017). Repealing the ACA without a replacement: The risks to American health care. Obstetrical & Gynecological Survey, 72(5), 263-264. Web.
Oberlander, J. (2018). The Republican war on Obamacare: What has it achieved? The New England Journal of Medicine, 3(1), 1-3.
Oberlander, J. (2019). Sitting in limbo: Obamacare under divided government. The New England Journal of Medicine, 4(1), 1-3.
O’Dowd, M. E., & Charbonneau, R. (Eds.) (2021). Junctures in women’s leadership: Health care and public health. Rutgers University Press.
Perricone, K. (2020). Barack Obama: His legacy of hope & change. Simon and Schuster.
Porche, D. (2021). Health policy: Application for nurses and other healthcare professionals. Jones & Bartlett Learning.
Raudenbush, D. T. (2021). Health care off the books: Poverty, illness, and strategies for survival in urban America. University of California press.
Rice, T., Unruh, L., Ginneken, E., Rosenau, P., & Barnes, A. (2018). Universal coverage reforms in the USA: From Obamacare through Trump. Health Policy, 122(7), 698-702.
Rice, T., Unruh, L., Rosenau, P., Barnes, A., Saltman, R., & Ginneken, E. (2014). Challenges facing the United States of America in implementing universal coverage. Bulletin of the World Health Organization, 92(12), 894-902. Web.
Rosenthal, M. S. (2020). Healthcare ethics on film: A guide for medical educators. Springer.
Rundio, L. (2021). Nurse managers’ guide to budgeting and finance (3rd ed.). Sigma Theta Tau International.
Shaw, C., Brown, A., & McCormick, J. (2021). After Obama: African American politics in a post-Obama era. New York University Press.
Stanhope, M., & Lancaster, J. (2021). Foundations for population health in community/public health nursing e-book (6th ed.). Elsevier Health Sciences.

